
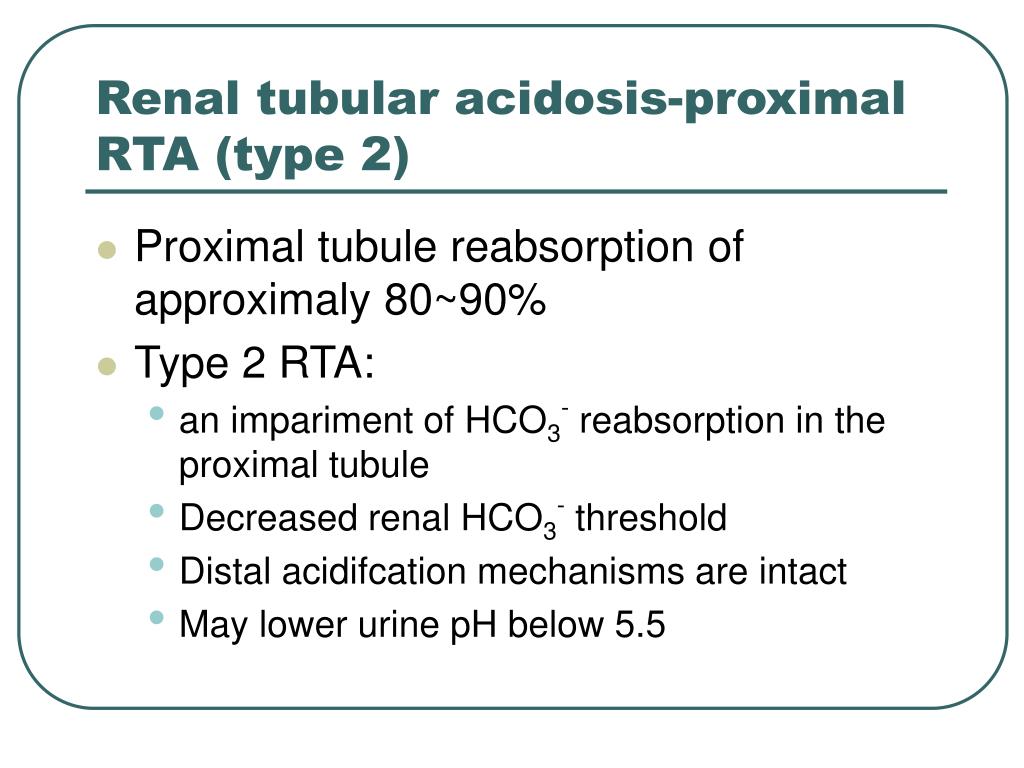
a HCO 3 – reabsorption in the proximal tubule. Schematic diagrams illustrating bicarbonate (HCO 3 –) reabsorption and regeneration in the kidney. HCO 3 – is also reabsorbed by a similar mechanism in the thick ascending limb of the loop of Henle (Fig. CO 2 is then freely absorbed across the proximal tubular membrane, where cytosolic carbonic anhydrase II catalyzes its reaction with water to form carbonic acid that rapidly breaks down to HCO 3 –, which is reabsorbed into the blood through the Na +/HCO 3 – cotransporter (NBCe1), and H +, which is then secreted back into the tubular lumen. HCO 3 – reabsorption involves secretion of H + into the proximal tubule through the Na +/H + exchanger 3 (NHE3) and H +-adenosine triphosphatase (H +-ATPase) transporters, after which luminal HCO 3 – reacts with secreted H + to form CO 2 and water, a process that is catalyzed by membrane-bound carbonic anhydrase isoform IV (Fig. The kidneys contribute to the maintenance of acid–base homeostasis by reabsorbing HCO 3 − in the proximal tubule, as well as regenerating HCO 3 – in the cortical collecting duct. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors. The clinical presentation, differential diagnosis, and management options for patients with RTA are also discussed. This review describes the physiological processes involved in the maintenance of normal acid–base homeostasis and provides an overview of the different types of RTA.
RTA occurs when the kidneys are unable to adequately reclaim filtered HCO 3 – or secrete sufficient hydrogen ions (H +) to maintain acid–base homeostasis. Renal tubular acidosis (RTA) develops as a consequence of impaired urinary acidification and is characterized by normal anion gap metabolic acidosis. Typically, an anion gap greater than 20 mmol/L may be considered as high anion gaps greater than 18 mmol/L should be further investigated.
Metabolic acidosis can have a normal or high anion gap, where the anion gap refers to difference between the number of cations (i.e., sodium and potassium ) and the number of anions (i.e., chloride and HCO 3 –). Metabolic acidosis is defined as an excess in non-volatile acid load that results in a primary decrease in plasma bicarbonate (HCO 3 –) associated with a low plasma pH. Metabolism of sulfur-containing amino acids (i.e., methionine and cysteine) yields sulfuric acid, while dietary phosphate yields phosphoric acid. The amino acids lysine and arginine are metabolized to generate acids, while metabolism of glutamate and aspartate and organic anions, such as acetate and citrate, yield alkali. In healthy individuals ingesting a typical Western diet, metabolism produces acid or alkali components, with a daily net acid production of approximately 1 mmol/kg of body weight per day. The maintenance of acid–base homeostasis is a major function of the body, accomplished by intracellular and extracellular buffering mechanisms, exhalation of carbon dioxide (CO 2) through the respiratory system, and acid excretion by the kidneys.

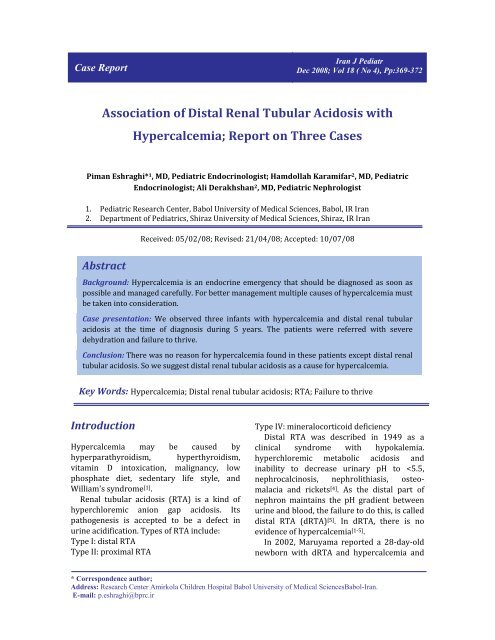
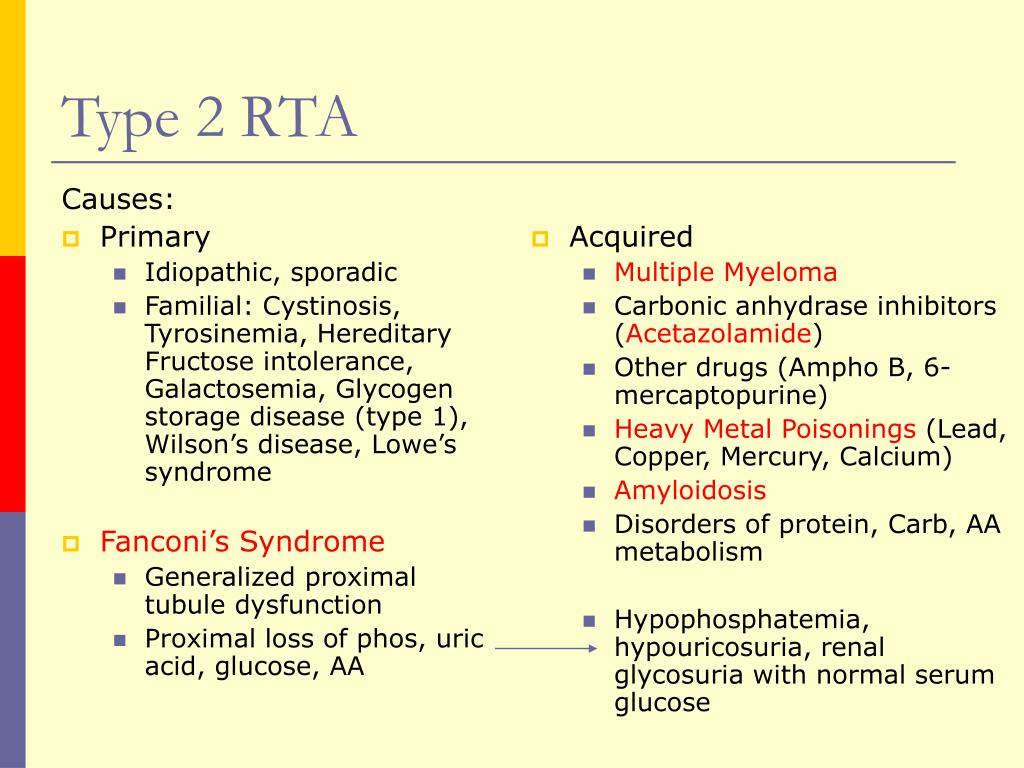
Treatment options include alkali therapy in patients with distal or proximal RTA and lowering of serum potassium concentrations through dietary modification and potential new pharmacotherapies in patients with hyperkalemic RTA including newer potassium binders. The diagnosis of distal versus proximal RTA involves assessment of urinary acid and bicarbonate secretion, while in hyperkalemic RTA, selective aldosterone deficiency or resistance to its effects is confirmed after exclusion of other causes of hyperkalemia. Accurate diagnosis of RTA plays an important role in optimal patient management. Type 3 RTA is a rare form of the disease with features of both distal and proximal RTA. The three major forms of RTA are distal RTA (type 1 characterized by impaired acid excretion), proximal RTA (type 2 caused by defects in reabsorption of filtered bicarbonate), and hyperkalemic RTA (type 4 caused by abnormal excretion of acid and potassium in the collecting duct). Using illustrative clinical cases, this review describes the main types of RTA observed in clinical practice and provides an overview of their diagnosis and treatment. Renal tubular acidosis (RTA) occurs when the kidneys are unable to maintain normal acid−base homeostasis because of tubular defects in acid excretion or bicarbonate ion reabsorption.


 0 kommentar(er)
0 kommentar(er)
